 In Part One of the series on how to treat tendon injuries, we considered the proper diagnosis of tendon disorders and how exercise and nutrition might contribute to injury recovery. In Part Two, we will examine additional treatment options.
In Part One of the series on how to treat tendon injuries, we considered the proper diagnosis of tendon disorders and how exercise and nutrition might contribute to injury recovery. In Part Two, we will examine additional treatment options.
Nutritional Supplements
In the previous article, I mentioned the importance of consuming high-quality, whole foods in order to optimize tissue health and encourage tendon healing. In particular, foods high in protein and rich in micronutrients should be emphasized. Beyond the food that you put on your plate, certain nutritional supplements may have a place in tendon injury recovery. We will examine several:
- Vitamin C – In the process of collagen formation, vitamin C acts as a critical cofactor, allowing enzymes to link amino acids together in a highly structured fashion. A study of Achilles tendon healing in rats demonstrated that high-dose vitamin C supplementation had stimulating effects on tendon healing due to modulation of blood flow and increased collagen synthesis.
- Glycine – A small amino acid found largely in bones, cartilage, and tendons, glycine is vital to collagen structure as it allows the collagen strands to pack tightly together. In America, very few of us consume bone, cartilage, and tendon products in our diets. As a result, there has been some concern that we may be relatively deficient in glycine and the case has been made that we should focus on consuming more glycine-rich foods in order to support collagen turnover and the production a number of important metabolites, some of which are involved in our body’s detoxification processes. In addition to mindfulness of glycine in my diet, I have been experimenting with taking 10 grams of glycine before my workouts due to some compelling research related to tissue health and recovery.
- Glucosamine, Chondroitin, Boswellia, Turmeric, Epigallocatechin Gallate (EGCG), and Nettle Leaf Extract – All of these have been shown to inhibit several chemical mediators and enzymes associated with inflammation and tissue destruction including nuclear factor-kappa beta (NF-kB), tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and matrix metalloproteinases (MMPs).
Medications
Though few pharmaceuticals are likely to positively influence tendon health in the long run, short-term use of various medications may have a role in treatment.
- Ibuprofen – Traditionally used as anti-inflammatory and pain relieving medication, ibuprofen may also act as a disease-modifying agent by inhibiting cell proliferation and the expression of certain proteins from the cell. One protein in particular, aggrecan, is a large proteoglycan that pulls water into a tendon and separates the collagen in early stages of tendon injury. As a result, use of ibuprofen for several days following acute tendon injury or pain may be a reasonable thing to consider.
- Nitroglycerine – Normally used to treat cardiovascular disease, nitroglycerine patches are being used in some cases of tendinopathy in order to increase cell turnover and blood flow. Their use is off-label, meaning that the FDA has not approved this drug for the treatment of tendon disorders. Additionally, there is no standard dosing, so effectiveness and side effects can vary according to the dose used. Typically, patients have to cut these patches into smaller pieces and then apply the patches over the affected area for at least 12 weeks to experience any noticeable change in symptoms. While you should check with your physician before considering this potential treatment, I have had success treating several patients and tendinopathies with nitroglycerine patches.
Manual Therapy
There are all sorts of manual therapies that have been suggested to speed tendon healing, ranging from gentle massage to aggressive, capillary-busting tendon “scraping”. While there is no great scientific evidence to support any of these treatment techniques, I seldom discourage people from trying them. Do they enhance blood flow, decrease “adhesions”, align collagen, or fortify the tendon structure? I dunno.
Manual therapy may also have a place in injury prevention. Generally speaking, we all get stiffer over time. Manual therapy might help with pliability, therefore preventing tendon dysfunction.
Corticosteroid Injections
The use of corticosteroid injections for the treatment of tendon disorders is controversial. Since corticosteroids can have deleterious effects on tenocytes, repeated injections may weaken a tendon, increasing the chance of a rupture or tear. Additionally, corticosteroid medications should never be injected directly into a tendon since this could conceivably increase the chance of tendon rupture. For this reason, I cringe whenever I hear of someone being treated with a steroid injection without use ultrasound-guidance.
While long-term benefits of steroid injections are debatable, they can be used to successfully decrease acute pain in order to enable someone to engage in therapeutic exercise to better facilitate recovery.
PRP is a regenerative therapy used to restart or accelerate healing. Here’s how it works:
- A simple blood draw is performed to collect a tube of blood
- Your blood is spun in a special centrifuge to separate and concentrate the platelets
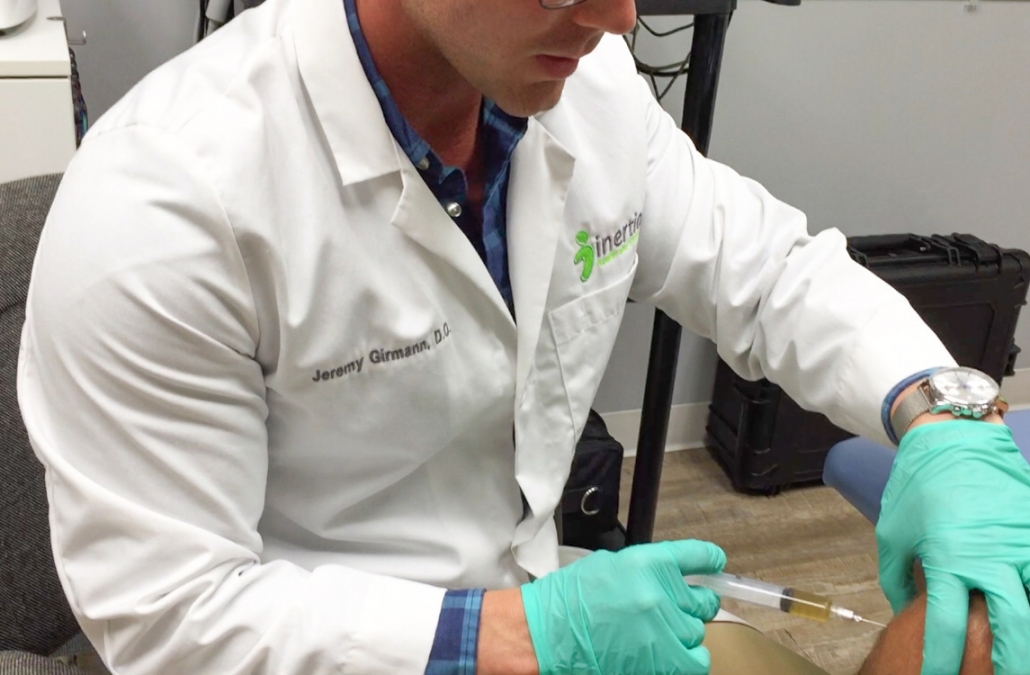
- The platelets are taken out of the sample and injected back into the site of injury or pain under ultrasound guidance
The platelets in PRP release many different growth factors that stimulate the natural healing process. In my practice, I’ve found that this treatment works particularly well for active and otherwise healthy individuals. I think that this is likely related to a few factors. First, you can imagine that the quality of PRP extracted from someone who eats well, doesn’t smoke, and exercises regularly is likely to be significantly different from that of someone who follows a burger n’ fries diet, smokes, and seldom leaves their couch. Also, I think that the microvasculature and collagen structure of active and healthy individuals disposes them to favorable outcomes.
Tendon Fenestration
As I often tell my patients, the body demonstrates somewhat of a “fix it and forget it” response to tendon injuries. Unfortunately, however, the “fix” is occasionally inadequate so we’re left with tendon problems that forgo further repair. Tendon fenestration involves using a needle to poke holes in the tendon under ultrasound-guidance (usually 40-100 punctures). Huh? Making Swiss cheese of a tendon might seem counterproductive but it’s quite beneficial in the setting of chronic tendinopathy. The local trauma causes bleeding and reinitiates inflammation, allowing the body to further fortify and heal the tendon tissue.
Just so you’re aware, local anesthetic is used to numb the treatment area prior to the procedure so patients actually experience very little discomfort with the fenestration.
Prolotherapy
Similar to tendon fenestration, prolotherapy is intended to reinitiate the healing process by injecting tissue irritants into the chronically injured or painful area. Most commonly, a dextrose (sugar) solution is used.

Stem cell therapy offers the potential to replace injured and degenerated tissue with tissue that is healthy and functional. Mesenchymal stem cell (MSC) therapy can be used to treat a number of musculoskeletal conditions. MSCs may help to recapitulate the appropriate signaling environment to encourage robust regeneration. We’re going to hear much more about stem cell therapy over the next several years.
Peptides
BPC-157 is an injectable peptide derived from a protein that has been identified in human gastric juice known as body protection compound (BPC). While it demonstrates robust protective properties in the stomach, BPC-157 has experimentally demonstrated protective and healing characteristics beyond the gastrointestinal tract. In rat studies of transected Achilles tendons, BPC-157 was shown to significantly accelerate tissue recovery. As a result, the researchers noted that gastric pentadecapeptide, BPC-157, may have a role in future tendon treatment.
While animal research shows promise, BPC-157 is not approved for human use and studies are needed to determine whether benefits extend beyond research animals. And though it is not approved for human use, perusal of online chat forums reveals that many people have in fact experimented with BPC-157 with hopes of enhancing recovery for a number of injuries, and positive outcomes have been reported.

These ultrasound images compare the right and left patellar tendons in a patient with left-sided patellar tendinosis. The degenerative changes cause enlargement of the tendon.
In the setting of chronic tendinopathy, regions of the degenerated tendon tissue often have a characteristic appearance when visualized with an ultrasound examination. When these regions of abnormal tissue cause lasting pain and dysfunction, removal of the damaged tissue may relieve symptoms. Whereas traditional surgical intervention used to be the exclusive option for tissue removal, new technology allows this to be done through a very small, needle-sized hole. During this procedure, the problematic area is visualized using ultrasound while a needle tip emits ultrasonic energy, ridding the tendon of the abnormal tissue. In my practice, this procedure has yielded excellent clinical results, even in cases of advanced tendon disorders.
Traditional Surgery
Due to the expanding number of non-surgical and minimally invasive treatments available for tendon disorders, traditional surgical intervention is becoming less and less common. For patients who experience acute tendon rupture or refractory tendon pain and dysfunction, surgical correction may ultimately be necessary.
As you can see, there are many available treatment options for tendon disorders. As a result, it’s important to consult with a qualified expert in order to help navigate the options and determine the most appropriate treatment.



