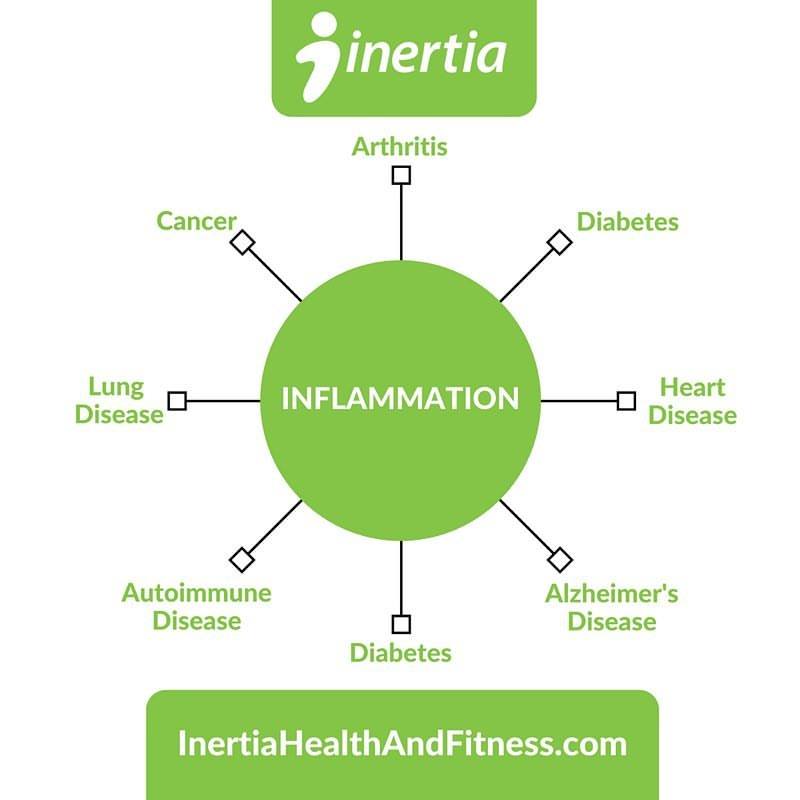
 When we study the causes of chronic disease, our investigations often reveal a usual suspect – inflammation. It is thought that inflammation plays a central role in the development of diabetes, cancer, heart disease, COPD, Alzheimer’s disease, autoimmune conditions, arthritis, and many other medical maladies.
When we study the causes of chronic disease, our investigations often reveal a usual suspect – inflammation. It is thought that inflammation plays a central role in the development of diabetes, cancer, heart disease, COPD, Alzheimer’s disease, autoimmune conditions, arthritis, and many other medical maladies.
Even so, inflammation is essential. It facilitates tissue repair. It heals broken bones after a fall and allows muscles to recover following an intense workout. In these cases, inflammation is acute and localized the area of injury. When inflammation becomes chronic and systemic, it can be particularly problematic. Consider fire. For thousands of years, humans have controlled fire to cook food and provide a source of warmth and protection. When fire gets out of control, it can burn through acres of land and destroy entire villages. It can serve us or scorch us.
Controlling inflammation is critical to maintaining optimal health. Let’s consider how this might be accomplished in a two-part series.
Exercise
As mentioned above, and as evidenced by sore muscles after a workout, exercise induces inflammation. This inflammation is, however, a transient and local response that occurs in the exercised muscles. Our bodies respond over time by fortifying the muscles and squelching the flames of systemic inflammation. Large population-based cohort studies consistently show an inverse association between markers of systemic inflammation and physical activity or fitness status.
 Body Composition
Body Composition
There is much that we have learned about body fat. Whereas it was previously thought that adipose tissue functions solely as a storage site for surplus calories, it has since been discovered that fat tissue releases a hundreds of molecules known as adipokines. Many of these adipokines, such as tumor necrosis factor-alpha (TNF-α) and leptin, demonstrate robust inflammatory activity in the body and have been linked to the perpetuation of many chronic diseases.
Sleep
Studies have demonstrated that individuals who experience sleep disturbance and shortened periods of sleep have elevated levels of inflammatory markers in their blood. While research is ongoing, some have proposed that this altered inflammatory status may be related to metabolic changes that occur with impaired sleep, as well activation of the autonomic system – the portion of the nervous system involved in the fight-or-flight response. But before you use this as an excuse to sleep the day away, also know that studies have similarly demonstrated an increase in inflammatory signals with extended sleep of greater than 8 hours.
Diet
Perhaps the most foundational factor in the day-to-day modulation of inflammation is diet. There’s a lot here so let’s ponder a few points.
We need to balance the fatty acids in our diets.
In most Western diets, omega-6 fatty acids such as linoleic acid are consumed in significantly greater quantities than omega-3 fatty acids. This creates an imbalance that can prove to be problematic. Fatty acids compete for various enzymes which convert them into molecules that can be either pro-inflammatory or anti-inflammatory. When an imbalance that favors omega-6 fatty acids is present, inflammatory molecules can be produced in excess.
 One of the causes of disproportionate consumption of omega-6 fatty acids is the considerable use of vegetable oils.
One of the causes of disproportionate consumption of omega-6 fatty acids is the considerable use of vegetable oils.
Have you ever noticed that vegetable oil isn’t actually derived from vegetables?
Corn – grain
Soybean – bean
Canola (aka rapeseed) – seed
Cottonseed – seed
Safflower – seed
That’s some pretty wild marketing that was intended to brand the oils as healthy.
So what are we to do? First, be mindful of how much “vegetable” oil you consume. In addition, consider increasing your intake of omega-3 fatty acids such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which are converted into a number of anti-inflammatory molecules. As written in the March 2016 article titled “Fish Oil and Omega-3 Fatty Acids”:
“I try to eat fish at least a few times each week. Fish (and therefore fish oil) are great sources of omega-3 fatty acids. In addition, I take 2 grams of omega-3 fatty acids in the form of fish oil each day. I consider this to be a sort of ‘insurance policy’ in case I’m not consuming enough through my diet. (Caution: Many products boast “1000mg of fish oil per pill”. Since only a fraction of the fish oil is made up of omega-3 fatty acids, you must often look closely at the supplement facts in order to determine the actual dose of omega-3 fatty acids in each pill.)”

We should avoid trans fats.
Most trans fatty acids are created through an industrial process that adds hydrogen to liquid vegetable oils. This results in the liquid oils becoming more solid, which extends the shelf life of processed foods such as cookies, crackers, creamers, and chips. Quite possibly the worse type of fat that we could consume, trans fats have been associated with an increase in a number of inflammatory markers and diseases.
We should cut the refined carbohydrates.
Refined carbohydrates are processed foods that have been stripped of much of the fiber and many of the nutrients that they originally contained. Examples include table sugar, fruit juice, bread, instant cereals, and pasta. These refined carbohydrates have been shown to directly increase the release of inflammatory molecules from immune cells. In addition, the marked rise in blood sugar that accompanies the consumption of refined carbs significantly increases the release of insulin from the pancreas. While insulin is needed to allow the blood sugar to enter cells, it also influences the activity of desaturase enzymes which convert the aforementioned linoleic acid into arachidonic acid and ultimately inflammatory eicosanoid molecules. To add insult to injury, the elevated blood sugar can also increase the production of free radicals which can further damage tissue.
The fiber found in unprocessed foods can limit the rise in blood sugar and can slow the release of insulin. Shoot for a daily goal of at least 30 grams of fiber from whole food sources.
Let’s summarize Part One.
What are some of the things that we can do to help control chronic, systemic inflammation?
-Improve body composition
-Exercise regularly
-Get between 7 and 8 hours of sleep
-Watch our intake of “vegetable” oil and boost omega-3 fatty acid consumption
-Avoid trans fats
-Decrease refined carbohydrates
-Consume at least 30 grams of dietary fiber per day


